We know that everyone has a very unique experience of the menopause. That’s why a tailored approach to menopause care is essential.
We always start our consultations by getting to know you and what you are experiencing. We explore how these symptoms are impacting life, love and work.
During your consultation, our specialist will discuss a range of evidence-based treatment options to help control your symptoms and will give you all the information you need to make an informed decision.
Using a holistic approach, we will cover everything from HRT and lifestyle, to relationships and cognitive behavioural therapy.
We will then create a bespoke treatment plan together that’s right for you.
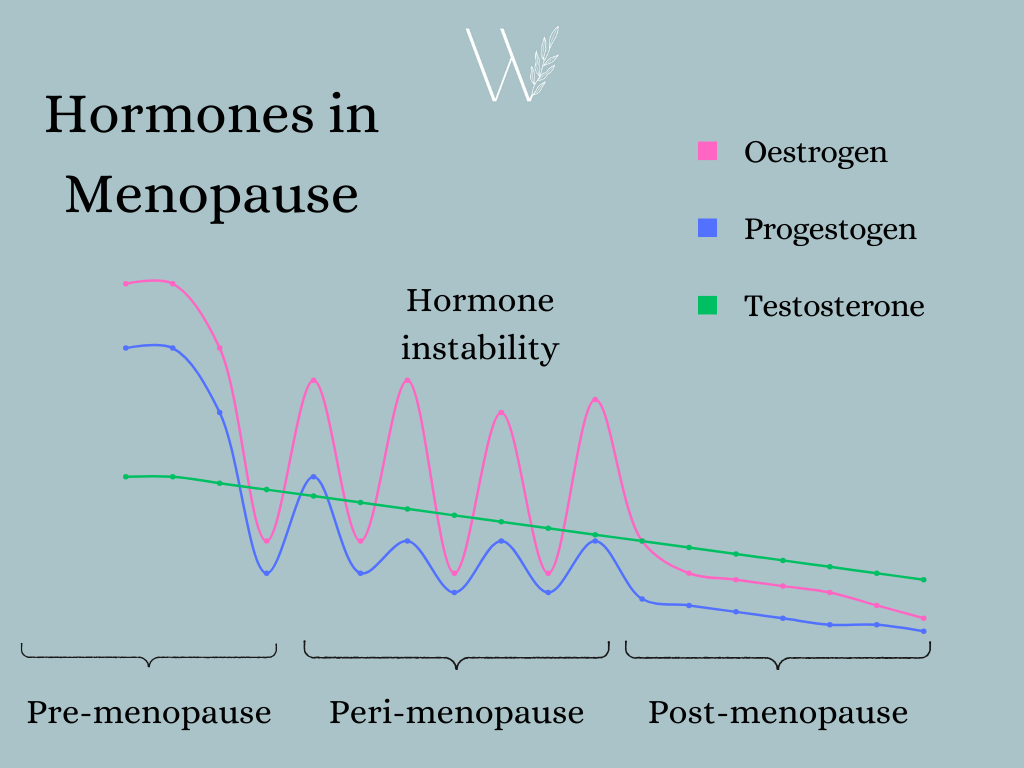
Prior to entering the menopause, we have 3 main natural hormones being produced by the ovaries: Oestrogen, Progestogens and Androgens (Testosterone). We start to enter the perimenopause when our ovaries stop releasing an egg regularly, and therefore less oestrogen is produced. This is leads to rollercoaster ride of hormone instability. You can feel fine one day and then full of symptoms the next. It is the instability of oestrogen that causes most menopausal symptoms.
The perimenopause typically begins a few years before our last period, though some women experience the perimenopause for up to 10 years prior to their periods stopping. The menopause is the time when it has been 1 year since your last period.
Our testosterone levels very gradually decline from our 30s: this can have an impact on some women. Find out more about testosterone.
For most experiencing perimenopausal symptoms, HRT can be the most effective treatment and is suitable in most cases. It provides hormone stability as well as treating the underlying hormone deficiency.
It also provides long-term benefits which is more crucial than ever due to our increasing life expectancy.
Unfortunately the risks of HRT have been over-stated, leading to a lot of anxiety about HRT. In reality, the risks of HRT are very low and the benefits far outweigh the risks in most cases. This is why it is so important to have an informed discussion about your individual risk with a menopause specialist.
The risk that concerns most people is breast cancer. There is a small risk of breast cancer for those taking traditional synthetic HRT. This risk slowly reduces when you stop HRT. The increased risk is similar to the risk of breast cancer in women who are overweight or who drinks 2 glasses of wine each day.
There are different types of HRT, such as body identical progesterone, which has been shown to be risk-neutral at 5 years of use.
Oestrogen-only HRT (used in those who have had a hysterectomy for example), has been shown to have little to no effect on breast cancer risk.
Taking oral HRT (oestrogen tablets) can increase the risk of blood clots and strokes. However taking oestrogen through the skin avoids this risk.
Taking oral HRT (oestrogen tablets) may carry a slight increased risk of gallbladder disease.
Read about the Women’s Health Initiative Study.
Body identical progesterone, or micronised progesterone is made from yams and mimicks your own body’s natural progesterone. This comes in the form of a capsule which you take at night, with the brand name Utrogestan. This type of progesterone has fewer side effects and risks when compared to traditional synthetic progesterone.
Beyond 5 years of use, the studies show that body identical progesterone may have a very slight increased risk of breast cancer, but much less than our traditional synthetic progesterone.
There is particular type of HRT (with a similar sounding name) that is provided from some private clinics. Compounded bioidentical HRT is produced by specialist pharmacies and it is an unregulated area. This is not recommended by the British Menopause Society as they are not evidenced-based for effectiveness and safety.
There is insufficient evidence to justify the multiple serum and saliva hormone tests claimed to precisely individualise compounded bioidentical HRT. The claims for bioidentical HRT are largely extrapolated from studies for body identical HRT, such as Utrogestan.
If you go through the menopause under the age of 40 (also known as Premature Ovarian Insufficiency – POI), it is extremely important to discuss HRT. Experiencing POI has significant health risks such as:
HRT significantly reduces these risks and is important to take until the age of 51, the average age of menopause. By doing this, we are just replacing the oestrogen your body would naturally produce until that age.
If HRT is not suitable, we can explore alternative options…
© 2023 Willow Health